
Guidance for Radiation Accident Management
Hospital Medical Management
Learn guidelines for the course of activity for hospital personnel responsible for managing the care of patients sent to the emergency department due to illness or injury caused by a radiological incident or accident.
Managing emergency care of patients contaminated with radioactive materials
If a hospital is notified that patients who are ill or injured in a radiological incident are en route to their facility, a planned course of action should be followed. The individual receiving the call should get as much information as possible, including the following:
- Number of patients
- Each patient’s medical status and mechanism of injury
- Whether this was an exposure or a contamination event
- If patients have been surveyed for contamination
- Identity of contaminant, if known
Depending on the size of the incident, the Hospital Incident Command System (HICS), or other standardized procedure, should be utilized. Small numbers of patients may be handled in a controlled area of the hospital. Mass casualty incidents may require more large-scale decontamination procedures, ensuring that medical/trauma triage and interventions take precedence.
Hospital emergency care of the radiation accident patient
Meet the radiation accident patient at the ambulance or at a triage area established near the treatment area.
During triage, life-threatening emergencies have priority over radiation urgencies. Once life threats are resolved, then consideration may be given to radiological issues.
Radiation injury rarely causes immediate signs and symptoms. Therefore, other causes of injury or illness must be considered.
Non-contaminated patients may be admitted into non-controlled areas.
Contaminated patients should be admitted to a specially prepared area, but medical and trauma care should not be neglected while contamination issues are addressed.
If the patient's condition allows, an initial, brief radiological survey can be performed to determine if the victim is contaminated. Any radiation survey meter reading above background radiation levels indicates the possibility of contamination. A more thorough survey should be performed once life-threatening problems are addressed.
The patient's contaminated clothing should be removed before arrival at the hospital (at the accident scene) if this can be accomplished without causing harm or delay in care. Otherwise, the clothing should be removed as promptly as possible (without compromising life or limb), using care to avoid the spread of any contaminants on the clothing. Clothing, and any accompanying sheets, blankets, or other materials should be placed in a plastic bag. Caregivers should change gloves after handling clothing or other potentially contaminated items.

Non-contaminated individuals can be cared for like any other emergency case. A specially prepared treatment area is not needed. Following attention to medical/trauma needs, question the patient to determine the possibility of radiation exposure from an external source. Remember, a person exposed without contamination poses no radiological hazard to caregivers.
Contaminated patients can have radioactive materials deposited on skin surfaces, or the contaminants may be internalized via ingestion, inhalation, or absorption. After examining the patient and identifying all injuries, a thorough radiological survey can be done.
A standard medical history should be obtained, including questions regarding any recent nuclear medicine tests. The patient may have anxiety related to the event and psychological support should be offered.
Certain clinical and radiological laboratory analyses (see Radiological and Clinical Laboratory Assessments section below) are essential to the care of the radiation accident patient. These laboratory tests are done to assess the biological effects of radiation injury; to identify abnormalities that might complicate treatment; to locate, identify, and quantify radionuclide contamination; and to provide information useful in accident analysis.

All samples must be placed in separate, labeled containers that specify name, date, time of sampling, and area from which samples were obtained. It is suggested that blood, urine, feces, or other samples taken during the emergency treatment period be retained for subsequent investigation. Samples that show no contamination should still be retained as pertinent negatives. Appropriate advice (radiation safety, legal, etc.) should be obtained regarding the storage and disposition requirements of collected samples.
| Samples needed | Why? | How? |
|---|---|---|
| In all cases of radiation injury: | ||
| CBC and differential STAT (follow with absolute lymphocyte counts every 6 hours for 48 hours when history indicates possibility of total-body irradiation) | To assess the radiation dose; initial counts establish a baseline, subsequent counts reflect the degree of injury | Choose a non-contaminated area for veni-puncture; cover puncture site after collection |
| Routine urinalysis | To determine if kidneys are functioning normally and establish a baseline of urinary constituents; especially important if internal contamination is a possibility | Avoid contaminating specimen during collection; if necessary, give the patient plastic gloves to wear for collection of specimen |
| When external contamination is suspected: | ||
| Swabs from body orifices | To assess possibility of internal contamination | Use separate saline- or water- moistened swabs to wipe the inner aspect of each nostril, each ear, mouth, etc. |
| Wound dressing and/or swabs from wounds | To determine if wounds are contaminated | Save dressings in a plastic bag. Use moist or dry swabs to sample secretions from each wound. For wounds with visible debris, use an applicator or long tweezers or forceps to transfer samples to specimen containers |
| When internal contamination is suspected: | ||
| Urine: 24-hour specimen | Body excreta may contain radionuclides if internal contamination has occurred | Use 24-hour urine collection container. If patient is being discharged, they should be provided a container for feces collection. A standard specimen cup is usually not sufficient. |
| Feces | ||
Some radioactive materials are corrosive or toxic because of their chemical properties. Medical attention may need to be directed first to the chemical issue if radioactive materials are components of acids, fluorides (uranium hexafluoride-UF6), mercury, lead, or other compounds.
In general, wounds should be decontaminated first, followed by body orifices, and then intact skin. The purpose of decontamination is to prevent or reduce internal contamination, to reduce the radiation dose from the contaminated site to the rest of the body, and to contain the contamination and prevent its spread.
In a contamination incident, any wound must be considered contaminated until proven otherwise and should be addressed prior to decontaminating body orifices and intact skin. When wounds are contaminated, knowledge of the radionuclide will aid in determining which target organ may be affected. Appropriate action is based on half-life, radiotoxicity, and the amount of radioactive material. It is important to consult REAC/TS as soon as possible and to initiate measures that prevent or minimize uptake of the radioactive material into body cells or tissues.
To control the spread of contamination, wounds should be draped, preferably with water-resistant material. Wound decontamination is accomplished by gently irrigating with saline or water. More than one irrigation is usually necessary. The wound should be surveyed intermittently. For accurate results, contaminated drapes, dressings, etc., should be removed before each survey. When surveying contaminated wounds, gamma radiation is easily detected while beta radiation may prove more difficult to detect. Without specialized wound probes, alpha contamination will likely not be detected. Following repeated irrigations, the wound should be treated like any other wound. If the preceding decontamination procedures are not successful, and the contamination level is still high, gentle debridement of the wound should be considered. Excision of vital tissue should not be initiated until expert medical or health physics advice is obtained. Debrided or excised tissue should be retained for specialized testing.
Debris, if visible, may be removed with forceps.
After the wound has been decontaminated, it should be covered. The area around the wound should be decontaminated as thoroughly as possible before suturing or other treatment.
Contaminated burns (chemical, thermal) should be treated like any other burn. Contaminants will slough off with the burn eschar. However, dressings and bed linens can become contaminated and should be handled appropriately.

Contaminated body orifices, such as the mouth, nose, and eyes need special attention because absorption of radioactive material is likely to be much more rapid in these areas than through the skin.
Nasal contamination may be lessened by allowing the patient to blow their nose. Do not irrigate the nasal passages, as this may force contamination further into the body.
Contaminated eyes should be rinsed by directing a stream of water from the inner canthus to the outer canthus of the eye while avoiding contamination of the nasolacrimal duct. Care should also be taken to not allow the run-off to collect in the ears.
Contaminated ears require external rinsing, and an ear syringe can be used to rinse the auditory canal, provided the tympanic membrane is intact.
Decontamination of intact skin is a relatively simple procedure. Complete decontamination, which returns the area to a background survey reading, is not always possible because some radioactive material can remain fixed on the skin surface. Decontamination should be only as thorough as practical.
Decontamination should begin with the least aggressive method. Take care to limit mechanical or chemical irritation of the skin. The simplest procedure is to wash the contaminated area gently under a stream of water (do not splash) using a soft cloth or surgical sponge. Warm tap water should be used. Cold water tends to close the pores, trapping radioactive material within them. Hot water causes vasodilation with increased blood flow to the area, opens the pores, and enhances the chance of absorption of the radioactive material. Aggressive scrubbing tends to cause abrasion and erythema and should be avoided.
If washing with plain water is ineffective, a mild soap (neutral pH) can be used. The area should be cleaned for 3 to 4 minutes, then rinsed for 2 to 3 minutes and dried, repeating if necessary. The contaminated area should be surveyed intermittently to see if radiation levels are decreasing. The decontamination procedure should stop when the radioactivity level cannot be reduced to a lower level or if skin irritation is beginning to occur. Expert advice might be needed to determine an appropriate stopping point.
Contaminated hair can be washed with a mild shampoo, taking care to not get it in the patient’s eyes, nose, mouth, or ears. Hair can be clipped if shampooing is ineffective and the patient agrees to have their hair cut. Shaving should be avoided since small nicks or abrasions can lead to internal contamination.
Ambulatory patients with localized contamination can be decontaminated using a sink or basin. If extensive body areas are contaminated, the patient can be showered under the direction of a radiation safety officer. Caution the patient to avoid splashing water into the eyes, nose, mouth, or ears. Repeated showers might be necessary, with clean towels provided for drying after each shower. Again, decontamination should be as thorough as practical.
A patient involved in a radiation incident may be anxious and should be provided explanations of procedures and actions being taken (isolation, use of survey meters, taking of samples, decontamination, etc.). Following emergent care, someone with a knowledge of radiation effects should spend adequate time answering the patient's questions and addressing their concerns.
Routine precautions for patient safety should not be forgotten. Be especially alert for potential falls or slips on wet floors, excessive heating or chilling, and electrical hazards.
In addition to routine medical documentation, descriptions of the incident, survey readings, samples taken, and the effectiveness of decontamination should be noted in the patient’s chart. Take care to note pre-existing conditions such as rashes, healing wounds, or scars. This information will be extremely valuable to medical consultants and health physicists in reconstructing the incident accurately and providing advice on further patient care.

A final head-to-toe radiological survey should be performed following decontamination procedures. Ambulatory patients may be surveyed at the control line. Non-ambulatory patients may be surveyed on a clean sheet and then transferred to a clean stretcher or wheelchair at the control line.
Providers should remove personal protective equipment (PPE) and be surveyed before leaving the controlled area. After the patient and providers have left the controlled area, a sign reading "CAUTION—CONTROLLED AREA—DO NOT ENTER" should be posted. Unless it is needed for emergency medical reasons, the decontamination area should remain secured until it can be surveyed and decontaminated, if necessary, by the radiation safety officer or other health physics expert.
Treatment of internal contamination
Once radioactive materials cross cell membranes, they are said to be incorporated. Incorporation is a physiological phenomenon related to both the physical and chemical natures of the contaminant. Incorporation can be quite rapid or it can take days to months. Thus, prevention of uptake is urgent but should not take precedence over life-saving interventions.
Several methods of preventing uptake might be applicable and can be prescribed by a physician. Some of the medications or preparations used in decorporation might not be available locally and should be stocked when a decontamination station is being planned and equipped.
Learn more about medications such as calcium-diethylenetriaminepentaacetic acid (calcium-DTPA), zinc-diethylenetriaminepentaacetic acid (calcium-DTPA), and Radiogardase (Prussian Blue).
Expert guidance is available from the National Council on Radiation Protection and Measurements (NCRP) Report 161 (Management of Persons Contaminated with Radionuclides).
If internal contamination is suspected or has occurred, samples of bioexcreta (24-hour urine and feces collection) should be obtained. Whole-body counting and radioassay can help evaluate the magnitude of the problem and the effect of any treatment.
Radiation injury
Exposure to penetrating radiation can involve the whole body or an isolated part of the body. The exposure can occur all at once (acute) or a little at a time (fractionated).
Cutaneous radiation injuries are often more localized and frequently involve the hands. These injuries seldom cause the classic signs and symptoms of the acute radiation syndrome.
Consider cutaneous radiation injury in the differential diagnosis if the patient presents with a skin lesion without a history of chemical or thermal burn, insect bite, or history of skin disease or allergy. If the patient gives a history of possible radiation exposure (such as recent medical diagnostic or treatment procedures using radiation), note the presence of any of the following: redness (erythema), blistering, dry or moist desquamation, hair loss (epilation), or ulceration. Local injuries to the skin usually evolve very slowly and symptoms may not manifest for days to weeks after exposure.
Conventional wound management may not be sufficient in these cases. Consultation with REAC/TS regarding definitive diagnosis, tissue dose, treatment, and prognosis is recommended.
Acute radiation syndrome (ARS) is an acute illness caused by exposure to higher doses of radiation to the whole body or a significant portion thereof. It follows a predictable course and is characterized by signs and symptoms which are manifestations of cellular deficiencies and the reactions of various cells, tissues, and organ systems to ionizing radiation. Immediate signs and symptoms require a larger, usually whole body, dose of penetrating radiation delivered over a short period of time. Penetrating radiation comes from a radioactive source or machine that emits gamma rays, X-rays, or neutrons.
The ARS is characterized by four distinct phases: a prodromal phase (mild symptoms), a latent phase (when signs and symptoms lessen or subside), a period of illness, and then recovery or, at much higher doses, possibly death. During the prodromal phase patients may experience nausea, vomiting, fatigue, and diarrhea. After extremely high doses, additional symptoms such as fever can occur. However, all of these symptoms may lessen or disappear in a day or two, and a symptom-free, latent phase follows, varying in length depending upon the magnitude of the radiation dose. A period of overt illness follows, and may be characterized by immune system compromise, electrolyte imbalance, problems with blood clotting, cardiovascular collapse, and sometimes altered levels of consciousness.
In general, the higher the dose the greater the severity of early effects and the greater the possibility of late effects.
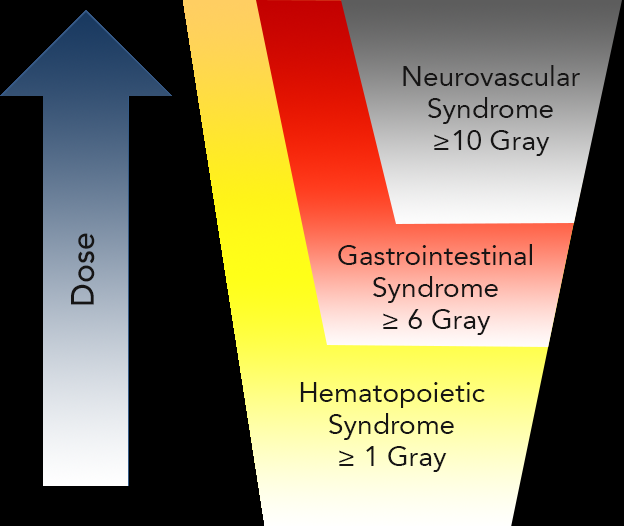
Depending on dose, the following syndromes may occur:
- Hematopoietic syndrome - characterized by deficiencies of white blood cells (WBCs), lymphocytes and platelets, with immunodeficiency, increased infection complications, bleeding, anemia, and impaired wound healing
- Gastrointestinal syndrome - characterized by loss of cells lining intestinal crypts and loss of mucosal barrier, with alterations in intestinal motility, fluid and electrolyte loss with vomiting and diarrhea, translocation of normal intestinal flora, sepsis, and damage to the intestinal microcirculation
- Neurovascular syndrome - primarily associated with effects on the vasculature and resultant fluid shifts. Signs and symptoms include vomiting and diarrhea within minutes of exposure, confusion, disorientation, cerebral edema, hypotension, and hyperpyrexia. May be rapidly fatal.
- Cutaneous syndrome - can occur with other syndromes (see above)
Diagnosis:
History of Exposure - Consider acute radiation syndrome in the differential diagnosis if there is:
- a history of a known or possible radiation exposure (for example, entering an irradiation chamber when the source is unshielded)
- a history of proximity to an unknown object that led to nausea and vomiting, especially if the nausea and vomiting cannot be explained by other causes
- a tendency to bleed (epistaxis, gingival bleeding, petechiae) and/or respiratory infection with neutropenia, lymphopenia, and thrombocytopenia, with history of nausea and vomiting two to three weeks previously
- epilation, with a history of nausea and vomiting two to three weeks previously
Symptoms - Type of symptoms, time of onset, severity, and frequency
Clinical Lab – Complete blood count (CBC) with differential. Repeat in 8 hours, then every 8 hours for 24 to 48 hours. Look for a drop in the absolute lymphocyte count. If the initial absolute neutrophil and platelet counts are abnormally low, consider the possibility that exposure may have occurred a few days to weeks earlier.

